
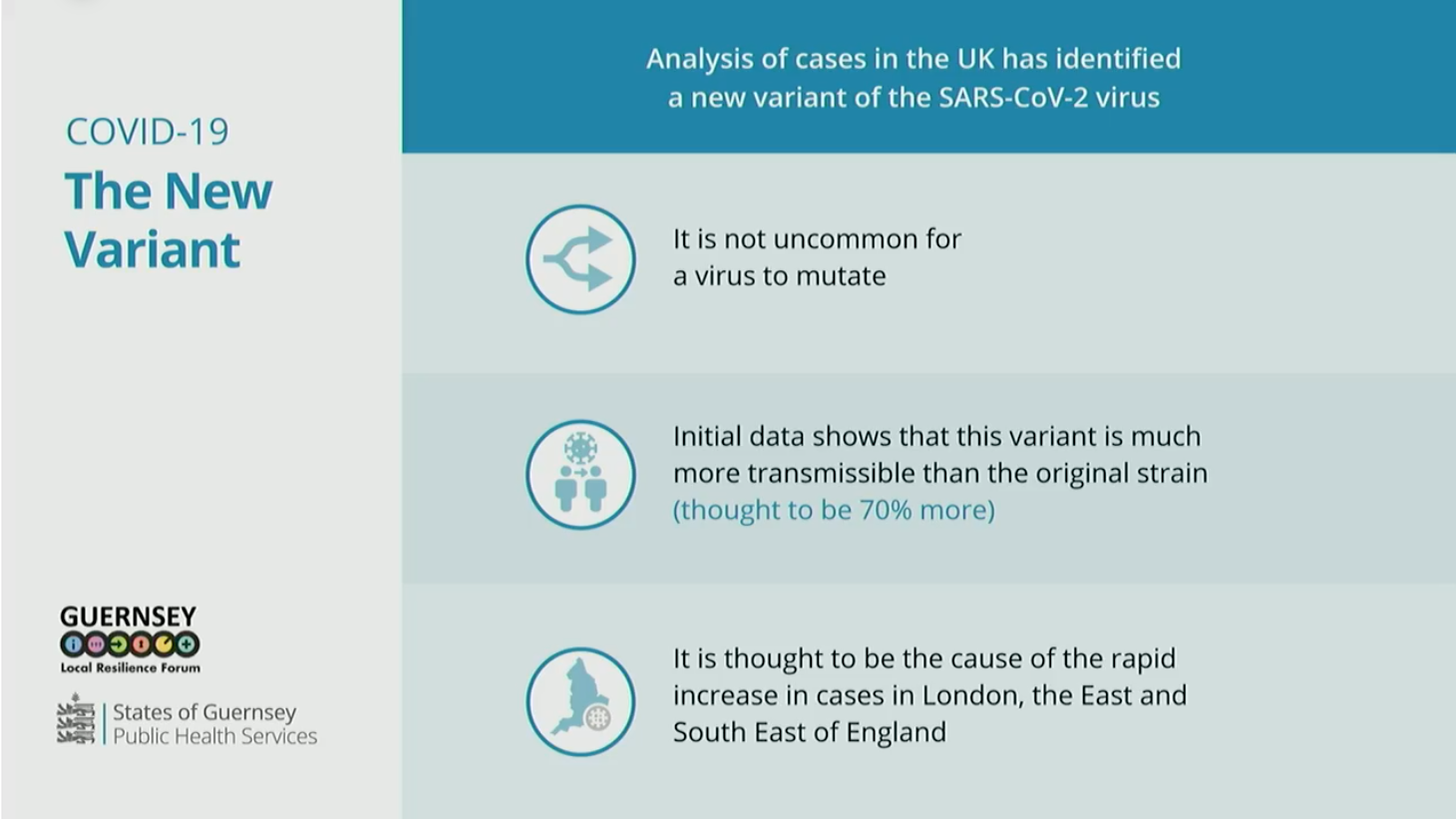
The emergence of a more transmissible variant of the corona virus was one of the key reasons behind the Civil Contingencies Authority's decision to go straight into lockdown when four cases of community seeding appeared.
It is not yet known whether any of Guernsey's recent positive cases of the virus contained a new variant strain that has been shown to be around 70% more transmissible than the original.
UK Prime Minister Boris Johnson has claimed it is also more deadly, however scientists linked to the study used by the PM have downplayed those suggestions, saying it is too early to draw such conclusions.
Public Health Director Dr Nicola Brink revealed that the emergence of variants had weighed heavy on the CCA's minds when the emergency-making body met on Saturday morning.
"The unknowns we are facing on this occasion are the emergence of the viral variants and exactly what that impact is going to be," she said, when asked about the key differences between last spring's lockdown and this one.
Pictured: Governments across the world are still learning about the new variant of Covid-19.
"That was key to our decision making; not only do we have these four cases, but we are sitting against the background of a changing situation.
"It was against that uncertainty that we have always done what we can to try to protect the health and wellbeing of the population."
While that doubt is a cause of continuing concern, Dr Brink said there are other "fundamental differences" that put Guernsey in a better position than we were 10 months ago.
"We understand more about Covid-19 as a disease and we understand more about the optimal management of it," she said. "We have a very well-established testing system.
"We went into lockdown on 25 March and our on-island testing capacity came in on 28 March. We were then able to test up to a couple of hundred samples a day but we are now able to test up to 1,000 cases a day, so we have a greatly enhanced testing capacity."
Pictured: Dr Brink said that face coverings are now strongly recommended, but not mandatory.
Health & Social Care President Al Brouard said a lot of groundwork was laid last year during efforts to get the PEH as ready as possible for a significant outbreak of the virus.
"The hospital is better prepared now, we have some idea of what to expect," he said.
"We have more ventilators, more oxygen available and there have been more protocols on how to manage it. We have the Brock Ward we can open within an hour if we need to if we get more cases that need serious treatment."
Other health and care services, such as the contact tracing on which the whole test, track and trace system depends, have evolved in light of new, local data.
Pictured: Contact tracers now go back 48 hours rather than 24, in order to catch as many contacts as possible.
"In the first wave of the pandemic we went back for 24 hours prior to people becoming symptomatic," said Dr Brink.
"We have reviewed the published data that has come out and we now go back 48 hours.
"The role of pre-symptomatic transmission - people transmitting the infection before they become symptomatic - also become apparent and that is really important, in fact it is more important than asymptomatic transmission."
"We have very focussed contact tracing which we had in the first wave of the pandemic but some broader more population-based testing to get a better handle of what’s going on."
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.