

To best understand the impact of Bailiwick Social Prescribing you need to look beyond numbers, trends and statistics.
What really shows the impact this model can have are the personal stories of how it has helped, they demonstrate something that cannot really be adequately measured.
Pictured: Bailiwick Social Prescribing Link Work Manager Trish De Carteret.
BSP Link Worker Manager Trish De Carteret recalled her work with a client who had had a stroke so could no longer drive. She was anxious and overwhelmed, everything was a problem.
She was becoming depressed because she could not go anywhere. She was scared to go on the bus.
What many people take for granted had become a barrier to living a healthy life.
So Trish worked with the client to build up her confidence and took a bus with her to Town - she had not been there for more than two years.
The idea was to pick up a Puffin Card and then go home, but in the end they went shopping and for a coffee.
That was the start of building confidence and eventually led to her taking part in the 30/30 walk to raise money to Les Bourgs, using the buses to travel all around the island and riding a bike by attending Wheels for You on a Sunday morning.
"It's not just one problem, one problem creates another problem, which creates another problem. That's the story of social prescribing quite often. But this lady's life has totally changed."
Bailiwick Social Prescribing was launched as a full pilot scheme in the summer of 2021.
Now, an evaluation of its effectiveness has created a positive picture that should help ensure its future.
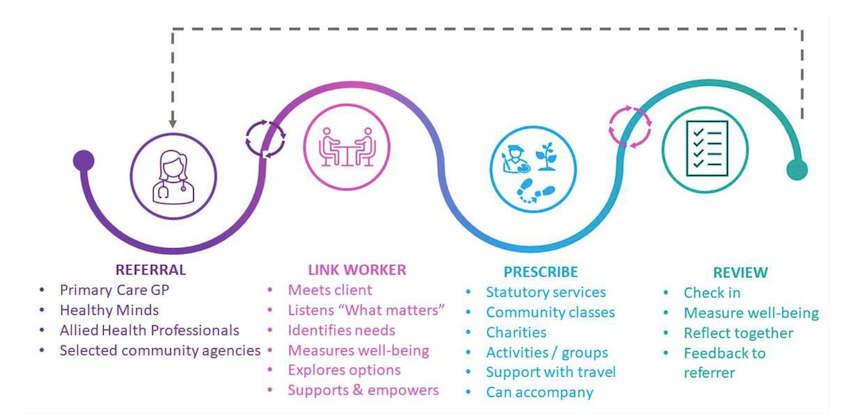
Clients are referred by GPs and some other professionals to the service and then link workers meet with them to understand their needs and connect them to a range of community organisations, charities, support groups and activities as well as statutory services that could help.
By the end of last year, BSP had partnered with 81 organisations/activities and a further 47 sports organisations.
They include health and financial support groups, community organisations, art groups, educational bodies and housing providers.
In a sign of how it is trusted and valued, small businesses now approach looking to help and this can have a wider knock on.
For example, All About Yoga now offers two classes where people just donate what they can afford, an initiative that stemmed from wanting to work with BSP.
Climb LBG changed their whole ethos around disabled climbing after their interactions with a BSP client.
BSP also commissions art, singing and Thai chi classes that anybody can attend, extending its impact into the community.
As part of her work with clients, Trish has found herself dancing in the dark and climbing up walls.
"You know what, if that's what the client needs, I can do that."
The BSP scheme was developed in collaboration between The Guernsey Community Foundation, Public Health and the third sector, work which began in 2019.
Since October 2020 it has been developed within the Health Improvement Commission, which employs the team of four link workers, who all work part time.
The Commission also provides background support with its staff and premises.
The Community Foundation provided funding from October 2019 to October 2023, when more backing was provided by the Social Investment Fund to the tune of £152,000 to keep the pilot running until the end of this year.
Public Health funds the salary of a part-time link worker and provides grants towards community classes, with further money coming from charity and the private sector to expand those.
Through all this, long-term funding has never been guaranteed.
But if this year's Budget is approved, money has been identified to ensure its future.
"Following presentation of the results of the report to the Committee for HSC, and their various decision-making groups earlier this year, we believe that funding to continue the BSP scheme has been built into the 2025 Budget (yet to be approved) which is very welcome news indeed," a spokesperson said.
"We are very grateful to both Public Health and HSC for their support."
Referrals to BSP are coming in thick and fast.
Up until the 31 December, there had been 695 - a number that has since broken through 900.
The figure has been rising each year, from 102 in 2021, to 228 in 2022 and 350 in 2023.
Until the end of last year the link workers had more than 6,300 contracts with clients, with 600 of those face to face.
The team only works with people over 18.
Their oldest client was 98, and there are others over 90 "who want to do more than sit in front of a TV all day".
Predominantly those referred to the programme are of working age, with a skew towards women, who account for 64%. 30% were unemployed and 13% received at least one type of benefit.
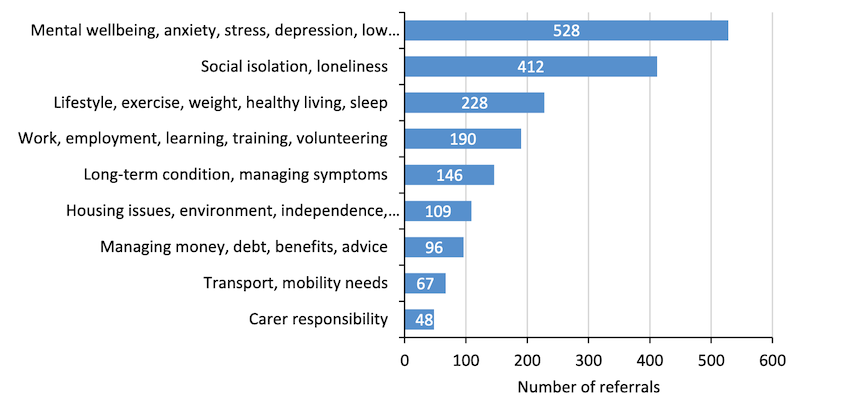
Mental wellbeing, social isolation, health behaviours, and employment were the most common client needs upon referral and for many there are a combination of needs.
"Social isolation and loneliness very, very sadly, affects every age group," said Trish.
"So we have people that are 18 who are lonely. They don't go out, they live behind their computer screens, and they don't have any interaction with anybody because they've left school and they're not working. So loneliness isn't just an old age thing, but there is a big gap in servicing Guernsey for people that are isolated under 60 with nowhere to go."
One of the problems faced by BSP is a waiting list.
As at 31 December there were 156 people waiting for help, with 14 of those having been referred 21 weeks ago, although inroads have now been made.
Assessing the waiting list since its launch shows that in the early days there was an average wait of one or two weeks, this climbed rapidly to 11 weeks March 2022 about where it has remained.
"The only negative feedback we had when we did the GP survey was that our waiting list was too long," said Trish.
"And I'm going to hand on heart we've had our waiting list longer than our funding was going to be in existence for.
"We have worked very hard, and full credit to the team on this. We changed our processes, we discussed the way that we deal with clients, and we have now got the waiting list down to a really realistic level, which is where we wanted it to be.
"So we're hoping now we've overcome that, but we have demand for the service that way outweighs our capacity.
"What we've had to do to get there is to stop the development of the scheme and concentrate purely on the clients, which is fine, but not sustainable going forward."
Pictured: Health Improvement Chief Executive Dr Simon Sebire.
In assessing the scheme, evidence was gathered from 213 people who had gone through the BSP, using both a broad measure of wellbeing and a more individualised approach about their personal concerns.
It showed that their concerns or anxieties were reducing.
And on average more general factors like happiness and life satisfaction were improving.
HIC Chief Executive Simon Sebire said that they had to be cautious about these results.
The trial was not randomised so it was not as simple as saying social prescribing was definitively causing these changes.
But when you looked at the data and the shifts it showed it started to build a picture that BSP was having a positive impact on people's wellbeing.
What people said was also indicative beyond the statistics.
"BSP has helped me a lot and brought fun back into my life"; "It's helped me increase my self-confidence and stopped me looking at my four walls every night"; "I wish I'd done sport years ago".
Success can also be about halting a decline.
"We must also remember at this point that when many people come to see our link workers, in the very first instance, their health is deteriorating," he said.
"They're already on a downward trajectory. So if they don't change and their score is zero. That's quite a good thing, because it's arrested this decline in people's well being. So we mustn't expect BSP to change people from one to a 10."
There is also evidence from GP surgeries about the number of appointments that people had in the year before they interacted with social prescribing, and the year after they had left.
61% of patients had fewer GP appointments in the 12 months after BSP compared to the 12 months before.
On average they were reducing by four GP appointments in that year.
"We can't prove that this is down to Bailiwick Social Prescribing, but when you look at it and you triangulate it against the qualitative data, the quantitative data... it starts to show that BSP is moving in the right direction. And I think this is a really, really important finding, because this is important not only for GPs, but it's important for patients, it's important for the economy and so forth."
GPs who responded to a survey about BSP were also supportive.
82% of them agreed that social prescribing should be a key feature of the primary care offering in Guernsey; 100% felt that their patients were more empowered for their wellbeing.
GPs think that 96% of their patients referred through BSP improved their physical health. While 88% felt it gave people the opportunity to reduce feelings of loneliness and isolation.
Dr Jo Le Noury said: "When we remember that a lot of the patients in our community now are really complex, they might not have just had a stroke, they might be diabetic, they may have financial difficulties. Bailiwick Social Prescribing has given GPs an opportunity to have something else in their armory to help support that individual's well being."
Pictured: Dr Jo Le Nory and Dr Nicola Brink answer questions about Bailiwick Social Prescribing.
Stare into a crystal ball and it is fair to say that without changes Guernsey's healthcare system will not cope.
A focus is needed on improving the health and wellbeing of islanders as current trends suggest hospital bed days could rise by 30% in the next two decades.
That is a figure based on modelling in Jersey, which is predicting 17,000 more annual hospital bed days, a similar exercise is being conducted here with a similar result expected.
What flows is the need for more staff, more community services and a bigger hospital, and that does not even begin to address the impact that it has on the individual, society and the wider economy.
"We need to consider really carefully how we look at developing and empowering people to stay healthy, what services we offer to promote the health and wellbeing of islanders," said Dr Nicola Brink.
"I think we need to look at what we are providing. Is it working? And the second thing is the value of partnership working, that whole island's approach, where we all work together.
"From my point of view, I see Bailiwick Social Prescribing as an integral part of the future provision of health and care to islanders and I would like to see it go on into the future."
It was important to acknowledge that government cannot fix everything, she said.
Services like social prescribing are often more agile, adaptable and can look at changing needs.
"I am so enthusiastic about social prescribing. It is a local program that has been developed for the local needs of islanders. This is not an off the shelf that we've taken from somewhere else, and just said, "let's see if we can get it to work across our islands".
Social prescribing is a non-medical model, helping respond to people's needs in a holistic fashion and helping to overcome some barriers to accessing health and social care.
It has all, Dr Brink argued, led to better outcomes for islanders.
Talk to those behind the BSP initiative and they will tell you it is not a silver bullet to all of Guernsey's health needs.
But evidence from the pilot shows that it is an important cog in the wheel to a holistic approach, with ripple effects that go out into the community.
With support the service could develop further.
More link workers would mean it could start taking self-referrals, for instance, potentially overcoming a barrier.
That extra staff capacity would also help address the waiting list.
More work needs to be done about awareness of the services, both so that people who are referred can be helped and that they also want to engage.
BSP could be expanded into Alderney.
There are also gaps that have been identified in the community groups and activities that are on offer in Guernsey, partially areas like social groups for young adults and low-cost evening and weekend activities.
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.