


Senior consultants from Guernsey's Medical Specialist Group have warned deputies that failing to progress with the modernisation of the island's hospital will result in longer waiting lists, worse recruitment, and poorer quality of life and care for patients.
A presentation was recently made to States members detailing why phase two of the Princess Elizabeth Hospital modernisation programme “should go ahead to safeguard patient care for the Bailiwick”.
It was revealed earlier this year that the projected costs for the outstanding work at the PEH has rocketed to over £150m.
But senior medics say fresh facilities are long overdue and could even hamstring the islands ability to deal with pandemics in the future.
Despite the huge leap in costs, Dr Steve Evans, MSG Chair and Consultant General Physician, said over the past two decades he has seen “more and more services crammed into a small building, making it very difficult to provide excellent healthcare to patients.
“So much time, effort and energy has been invested in this project. We have worked out the details of room sizes, transfer times, walked it all through, and we have a great contractor on site with invaluable experience of working in a healthcare environment.”

Pictured: Phase One of the rebuild is underway.
Mr Evans added that major new facilities across the hospital site are “vital to recruitment”.
“If we are to attract high calibre medical specialists in an incredibly competitive market, they have to know they are coming to an island which values and invests in healthcare.”
This was echoed by Michelle Le Cheminant, a Consultant Anaesthetist, who said when she took her job in 2019 the agreed hospital modernisation provided a reassuring “clear vision and credible strategy to deliver high quality, sustainable healthcare”.
“Healthcare workers need to feel valued and achieve job satisfaction, which means delivering high quality care for patients and to do that we need the right facilities. The alternative is burnout, worsening recruitment challenges and ever-rising agency staff costs”.
Lauren Green, Consultant Obstetrician and Gynecologist also said that “part of the attraction was the planned modernisation of women and children’s facilities,” when she arrived in Guernsey in 2021.
“The current maternity set up with no immediate access to an obstetric theatre presents a significant risk to local families and staff.”
“Even as a local, I would have reconsidered my application had modernisation of facilities not already been underway. We want to deliver the best care possible, and need to be supported with the facilities to do so otherwise we risk significant issues.”
Medical Oncologist, Dr Matthew Clark agreed: “I was hugely impressed by the foresight and the understanding of what’s needed. It was a big factor in me coming here, thinking about how over the next 20 to 30 years we can really deliver fantastic care for islanders”.
Dr Clark added that jurisdictions such as Singapore and Norway recognised the impending demographic changes and have invested to meet the future requirements.
The States of Guernsey estimates that the number of people over 65, who will require more frequent and complex medical interventions, will increase to 25% of the population by 2050.
Ms Le Cheminant also cited the British Journal of Surgery, which recently predicted that one in five over the age of 75 will require surgery each year by 2030.
“Local waiting lists in endoscopy and orthopaedics remain high and Phase Two provides much needed additional theatre capacity for both areas,” she said. “A huge number of additional procedures for an elderly, frail population with multiple health problems will place strain on already stretched services.
“Additional theatre capacity also provides a much-needed all-day emergency theatre so urgent surgical work, often for elderly patients, can be done in daytime hours.
George Cooper, Orthopaedic Surgeon, said while length of stay locally is “excellent” compared to the UK it is now at capacity with waiting lists that won’t improve.
Phase Two would see a second theatre for hip and knee replacement built, which would ensure an income stream from private appointments to the hospital, he added.
“So, if it will cost society more if we don’t increase hip and knee replacement capacity, if people will suffer for longer without more theatres and if they lose income – how can Phase Two be reasonably rejected or delayed?”
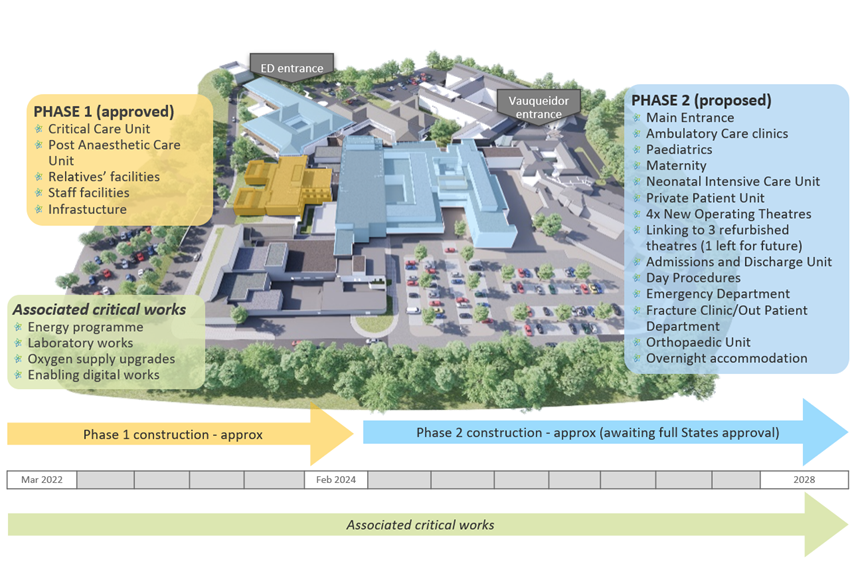
Pictured: Phase Two of the project promises the most significant changes.
Other MSG staff said the current facilities will not keep pace with the forecast increase in patient demand, are ageing, and result in undignified care for patients.
Ms Green said women requiring a sudden caesarean have to travel past multiple wards, down long corridors and take a lift to the theatre. This is unlike any other unit she has worked in.
“Our current [maternity] ward environment is no longer fit for purpose. Privacy, dignity and respect are pillars of the care we aim to provide. At present we do not have en-suite facilities for labouring women. It is difficult to provide the care we aspire to when having to ask women to share a toilet.”
Dr Kate Allen, Physician and Diabetologist, said the planned revamp of the outpatient services would unify several teams which help manage the treatment of around 3,000 people living with diabetes.
“It’s frustrating, because I know how much better the quality of life could be for people living with diabetes if we could work in this multi-disciplinary way,” she said.
Dr Clark also relayed a sense of “anger and dismay” from Jersey health professional who have dealt with several years of delay and change in their hospital rebuild project. To date no spades have entered the ground and hundreds of millions have been spent.
He said there was a “sense of disbelief that Guernsey might pull the plug on a much-needed hospital modernisation that is all ready to go ahead”

Pictured: Senior medical and States staff claim the hospital is not suited to dealing with infection control.
Ms Le Cheminant said covid-19 highlighted that better preparation for future pandemics is essential.
The pandemic review, published by the States of Guernsey yesterday, also showed that the hospital struggled to increase the number of beds within the existing building in a way that would ensure infection control due to poor layout.
“Phase Two helps us do this with isolation rooms in maternity and paediatrics and the flexibility to repurpose facilities,” Ms Le Cheminant said.
Ms Green echoed this: “Our day patient unit is located at the far end of the maternity ward, meaning that attenders need to walk past the entrance to labour ward and the inpatient beds. This is difficult in maintaining privacy and infection control, especially during the pandemic”.
LISTEN: Believing the ‘false narrative’ could stop Guernsey’s Education Programme
Hospital plans to be put on ice under P&R's bid to save money
HSC President vows to fight for hospital funds
Hospital project could hit £154million - more than double original estimates
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.