

Guernsey's lack of 24-hour crisis care for people who need mental health support is one of a number of gaps in the island's care system.
This comes as part of a report Mind UK have compiled following a survey in June of more 1,023 mental health service users and 126 professionals, all of whom provided information about their experiences with services across the primary, secondary and voluntary sectors.
Guernsey Mind commissioned the survey to help it be better informed as to people's opinion on the island's service.
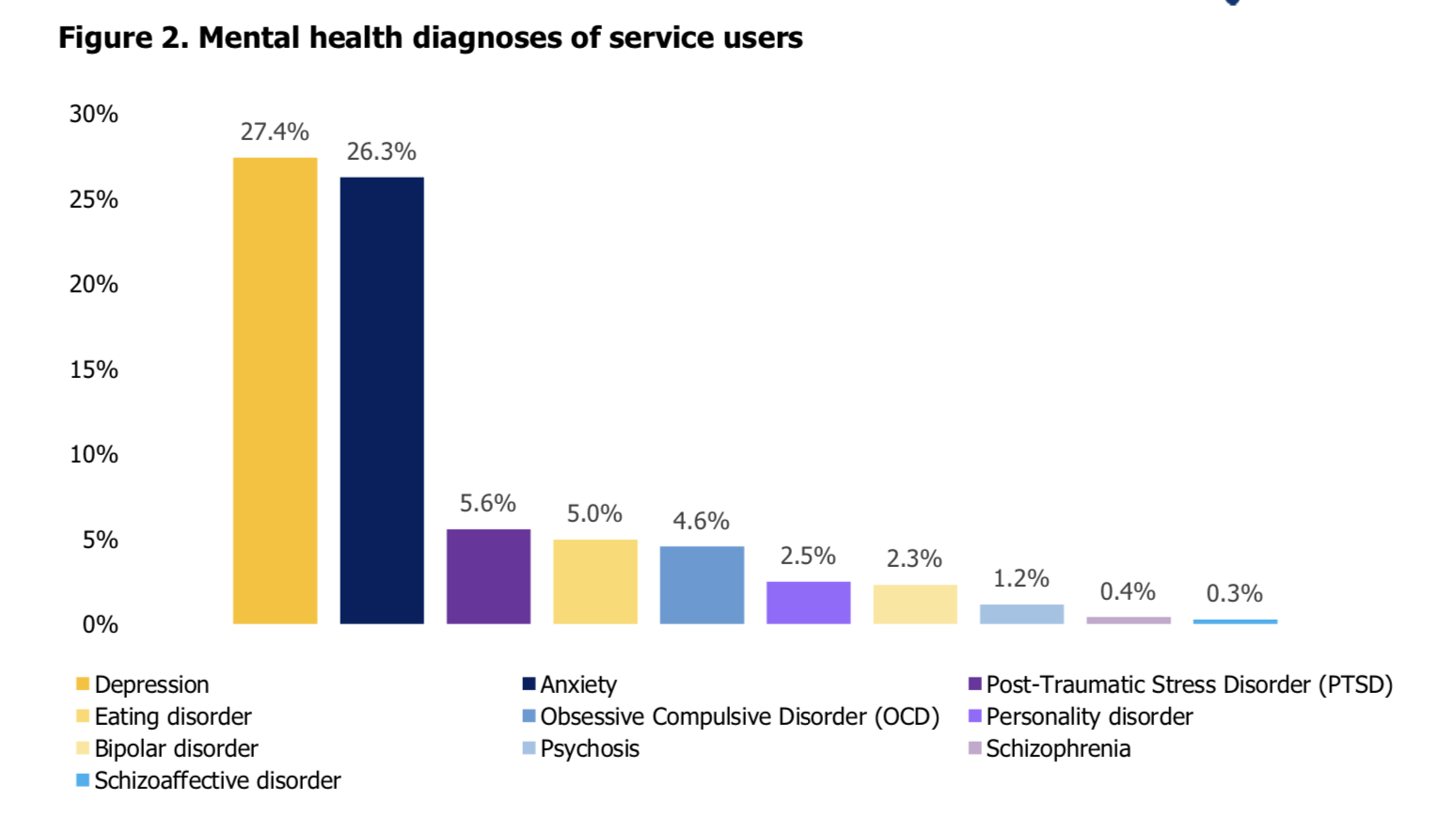
Pictured: A breakdown of diagnoses across service users.
The research revealed a mental health system that is working hard to support people but facing severe pressures from an increasingly large and complex case load, staff recruitment challenges, training gaps, limited opportunities for service user feedback, and a lack of joined up working between the sectors.
Pictured: A number of quotes from service users and service professionals were included in the report.
Further, it pointed to a lack of 24-hour crisis care, long waiting lists to access secondary care, gaps in discussing medication and side effects and a failure to provide an opportunity for feedback across all sectors as some problems that need addressing.
All-in-all, the report made 17 recommendations which aim to improve the provision of mental health services across the Bailiwick. They are listed below.
Emily Litten, Executive Director of Guernsey Mind, welcomes the positive and action focused tone of the report. "It has been very difficult for us to understand the needs of people locally, we have been playing a guessing game in terms of whether people are happy with the services they are receiving, and the choices that they want to have about their care. With so many people responding to this survey we know that people care passionately about the services they are receiving, they want change and they want their voices to be heard," she said.
"The Wellbeing Survey for Guernsey and Alderney 2018 showed that 27% of over 50’s and 45% of under 50’s described themselves as experiencing large amounts of stress. Furthermore, 28% of over 50’s and 35% of under 50’s living in Guernsey describe themselves as being intensely socially lonely. Our mental health needs are more important than ever, and we need to listen to the community voice and work together to do better."
Overall, the report found that experiences of primary care and voluntary sector mental health services are very positive whilst experiences of secondary care services are more negative. There is also a need for better quality information provided by all types of services and professionals need greater support to look after themselves and the people they work with. The need for better collaboration between sectors is a main finding of the research.
At present there is no 24-hour crisis cover and the report says that having nowhere to go in a crisis situation may explain the increase in severe and complex presentations of people who are coming into services because they are not receiving the support when they are no longer able to cope by themselves.
44% of service users felt the wait to access secondary care was longer than expected. Once service users gained access to secondary care services, just over half felt that the care met their needs. This was much lower than primary care and the voluntary sector, who both met 84% of client needs. Managing referral processes, giving patients enough information about medication, and involving people in decisions about their care, especially discharge planning, emerged as substantial issues for secondary care.

Pictured: Deputy Heidi Soulsby, President of HSC, with Nicola Brink, the Director of Public Health.
Mental health care professionals are also found to be in need of support. Only 40% felt supported in their workplace and 44% felt their role had had a negative effect on their own mental health. Despite high numbers of professionals experiencing mental health problems 72% had taken no sick leave in the last 12 months.
Deputy Heidi Soulsby, the President of HSC, said: "We welcome the survey by Guernsey Mind and the views of service users is incredibly helpful to us. We’re pleased to see positive feedback with regard to the primary care services we provide. While secondary care faces greater challenges, we should recognise that the majority of service users were positive about the care they receive. That’s down to the hard work of all our staff who, as the report recognises, face a growing and increasingly complex workload. We will now take time to look over the recommendations in detail to see how best we can deliver them. However, we can confirm that since the survey, Health & Social Care has been accepted as a signatory to the Prevention Concordat for Better Mental Health and undertaken a gap analysis of services which resulted in us requesting funding for the development of a mental health and wellbeing centre.
"With regard to the role of the voluntary sector and the need for more information and a more joined-up approach, collaborative working is a key principle of the new model of care and Mind is a member of the steering group overseeing the implementation of the Mental Health and Wellbeing Plan. How much further we can go is dependent on funding and resources and, as we’ve highlighted previously, the demands across HSC are rapidly increasing and funding is no longer enough to provide the level of care the community expects. It is time for a bigger public discussion about what people are able and willing to pay."
Ms Litten concluded saying that implementing all of the recommendations will "improve the quality of information available, increase collaboration between services, support the wellbeing of staff, and empower people to make choices about their care.
"In June the States of Guernsey unanimously agreed to a HSC amendment to the P&R Plan to invest in a Mental Health and Wellbeing Centre for Guernsey. This is the starting point for collaboration between sectors, incorporating social prescribing, a move to 24/7 support and better mechanisms for collaborative discharge planning and collecting feedback. We look forward to working together to build an even more productive, compassionate and connected community," she said.
Pictured top: The Oberlands Centre, where much of the island's mental health system is located.
Comments
Comments on this story express the views of the commentator only, not Bailiwick Publishing. We are unable to guarantee the accuracy of any of those comments.